Introduction
Drowning represents a critical public health issue, causing approximately 236,000 deaths annually worldwide, making it the third leading cause of death from unintentional injuries globally. In the United States, the average number of deaths due to unintentional drowning exceeds 4,000 per year, with specific populations, such as children aged 1 to 4 years, being particularly at high risk.(The Latest Drowning Statistics n.d.)
In 2002, the World Health Organization defined drowning as “the process of experiencing impaired breathing as a result of immersion in a liquid.”(Organization 2023)
This case highlights the importance of prompt recognition and immediate treatment of respiratory distress resulting from a drowning incident. The use of non-invasive ventilation, such as continuous positive airway pressure (CPAP), and early antibiotic therapy can play a pivotal role in stabilizing the patient’s condition and facilitating potential recovery. Continuous monitoring and support in such cases are essential to prevent complications and ensure a positive outcome.
Near drowning accidents can result in critical respiratory complications from water inhalation, causing acute respiratory distress similar to acute respiratory distress syndrome (ARDS). Factors contributing to the occurrence of acute respiratory distress include increased vascular permeability, inflammation of pulmonary tissue, and fluid accumulation within the alveoli. These factors result in impaired gas exchange and low blood oxygenation; for example, increased vascular permeability allows fluid to leak into the alveoli, while inflammation further disrupts effective oxygenation. In this report, we review the clinical case of a 16-year-old patient who arrived at the emergency department with respiratory distress after an almost complete drowning accident. Treatment strategies included high-flow oxygen intervention, antibiotic use, as well as non-invasive ventilation.(Siegel MD 2024b)
Clinical case presentation
Patient Data
- Age and gender: 16 years old, male
- Medical history: No known prior medical history documented
Main complaint:
Difficulty breathing and respiratory distress after an almost complete drowning incident in a pond.
History
The main reason for acceptance:
The patient arrived at the emergency department after suffering an almost complete drowning accident in a pond, where he had been submerged underwater for an unknown period with loss of consciousness. The family reported that the patient had difficulty breathing and respiratory distress that began several hours after the incident.
Initial symptoms on arrival
- Difficulty breathing and severe respiratory distress.
- Complete loss of consciousness during drowning, recovering before arriving at the emergency.
Clinical examination
- Nervous system: The patient was alert and responsive to stimuli, with a Glasgow Coma Scale (GCS) of 15/15.
- Respiratory system: Soft crackles were heard bilaterally in the lung fields.
- Cardiovascular system: Heart sounds (S1 and S2) were regular with no murmurs.
- Digestive system: The abdomen was soft and non-tender.
- Pupils: Reactive to light bilaterally.
- Limbs: No noticeable edema or abnormalities were observed.
- Vital signs: Blood pressure was 100/60 mm Hg, pulse was 123 bpm, oxygen saturation was 78% on ambient air, and blood sugar was 90 mg/dL.
Diagnostic tests
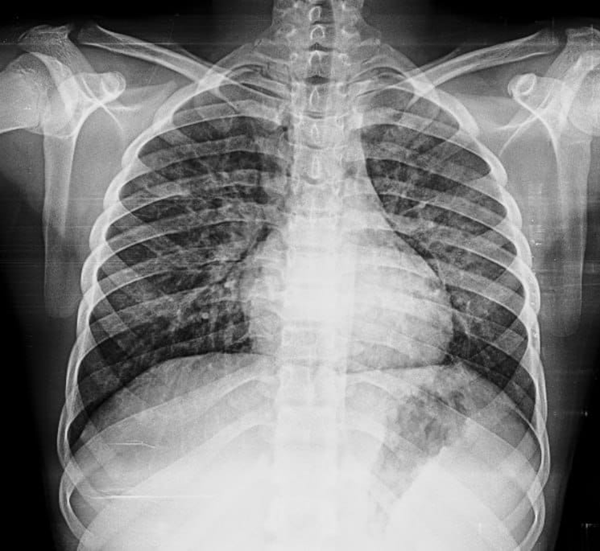
- Simple chest X-ray: Showed bilateral pulmonary infiltrates.
- Electrocardiogram (ECG): Sinus tachycardia.
- Laboratory blood tests:
- o Leukocytes (WBC): 15,400 cells/μL (normal: 4,500-11,000 cells/μL), indicating a moderate increase suggestive of inflammation.
- o Other tests: Within normal limits, except for an elevated C-reactive protein (CRP) of 112 mg/dL (normal: < 10 mg/dL), indicating inflammation.
- Electrocardiogram (ECG): Sinus tachycardia.
List of laboratory tests
| Parameter | Result | Normal Range |
|---|---|---|
| White Blood Cells (WBC) | 15,400 cells/µL | 4,500-11,000 cells/µL |
| Hemoglobin (HGB) | 13.6 g/dL | 13.5-17.5 g/dL for males |
| Platelets (PLT) | 167,000 cells/µL | 150,000-450,000 cells/µL |
| Creatinine | 1.0 mg/dL | 0.7-1.3 mg/dL for males |
| OLD | 34 U/L | 7-56 U/L |
| C-Reactive Protein (CRP) | 112 mg/L | <10 mg/L |
| INR | 1.1 | 0.8-1.2 |
| Chloride (Cl) | 103 mEq/L | 96-106 mEq/L |
| Potassium (K) | 4.8 mEq/L | 3.5-5.0 mEq/L |
| Sodium (Na) | 135 mEq/L | 135-145 mEq/L |
| Lactate | 2.3 mmol/L | 0.5-2.2 mmol/L |
| HCO3- | 22.3 mEq/L | 22-28 mEq/L |
| Creatine Phosphokinase (CPK) | 224 U/L | 30-200 U/L |
| Urine Analysis – Red Blood Cells (RBC) | 2-4 cells/HPF | 0-3 cells/HPF |
| Urine Analysis – White Blood Cells (WBC) | 50-60 cells/HPF | 0-5 cells/HPF |
| Arterial Blood Gas (ABG) – pH | 7.42 | 7.35-7.45 |
| Arterial Blood Gas (ABG) – Po2 | 54 mmHg | 75-100 mmHg |
| Arterial Blood Gas (ABG) – Pco2 | 34.8 mmHg | 35-45 mmHg |
Initial diagnosis:
Based on the clinical presentation, physical examination, and initial investigations, the initial diagnosis was identified as a drowning-related lung injury, consistent with mild acute respiratory distress syndrome (ARDS).
Therapeutic intervention
Emergency measures
Airway management:
The patient’s airway was clear as the patient was conscious. Given the low initial oxygen saturation of 78% on ambient air, a mask with a high-flow oxygen reservoir bag (delivering 10-15 L/min) was utilized to ensure adequate oxygenation.
Fluid resuscitation:
Two large-bore intravenous lines were established, and intravenous fluids were administered to maintain hemodynamic stability.
Non-Invasive Ventilation
After failure to achieve sufficient improvement in oxygenation using the mask with the reservoir bag, it was decided to initiate continuous positive airway pressure (CPAP) therapy at a frequency of one session every two hours to enhance ventilation and reduce respiratory stress. The CPAP was set with the following parameters: PSV 10, Itriger 2, Rise-T 4, PEEP 6.
Drug Therapy
Antibiotics: Treatment with Meropenem was initiated to cover the high risk of aspiration pneumonia due to drowning. Meropenem was chosen for its broad-spectrum coverage against both aerobic and anaerobic bacteria, as well as its proven efficacy in treating inhalation-related pneumonia.(Pacifici 2024)
Preparation for intubation when needed with constant monitoring.
Follow-up
The patient’s condition was carefully monitored in the Intensive Care Unit with close follow-up of vital signs and oxygenation levels. The patient showed a gradual improvement in oxygenation levels after repeated use of the CPAP machine, with a gradual decrease in heart rate and an improvement in oxygenation (reaching 94%) 24 hours after the start of treatment.
On the third day of treatment, the patient’s condition showed remarkable stability, allowing for a gradual reduction in CPAP dependency. Vital signs improved significantly over time, and oxygen levels returned to the normal range without the need for additional oxygen support.
A new chest X-ray was performed to assess the improvement, revealing significant progress in the pulmonary condition. Laboratory tests also demonstrated a gradual decrease in C-reactive protein (CRP) levels to 34 mg/dL, and a normalization of the leukocyte count to 9,400 cells/μL, indicating marked improvement in the aspiration pneumonia.
Discharge and Follow-up Recommendations
On the fourth day, after ensuring the stability of the patient’s condition through a final examination, it was decided to discharge the patient with clear directions for follow-up in the outpatient clinic to complete the recovery process. The recommendations included:
- Periodic follow-up in the clinic: To monitor the progress of breathing and identify any possible complications.
- Avoid water activities: Until the lungs are completely healed, in order to avoid any future complications.
- Psychological support counseling: To assess any psychological effects of the incident and provide necessary support, particularly to prevent the development of post-traumatic stress disorder (PTSD).
- Psychological support counseling: to assess any psychological effects of the incident and provide the necessary support, especially to avoid the development of post-traumatic stress disorder (PTSD).
Conclusion
This case highlights the importance of rapid intervention and integrated treatment in cases of near drowning, particularly in managing acute respiratory distress. The use of non-invasive ventilation and early antibiotic therapy can play a pivotal role in improving treatment outcomes and ensuring sustainable stabilization of the patient.
Acknowledgment
This case was treated at Al-Quds Hospital of Hand in Hand for Aid and Development” (HIHFAD), and the case was followed up by Dr. Abdul Razzaq Hilal, resident in internal medicine, under the supervision of intensive care and chest specialists Dr. Muhammad Dallah and Dr. Ammar Kaysum.
References
Organization, World Health. 2023. “Drowning.” https://www.who.int/news-room/fact-sheets/detail/drowning.
Pacifici, Gian Maria. 2024. “Clinical Pharmacology of Meropenem.” Biomedical Journal of Scientific & Technical Research 55(2). doi:10.26717/bjstr.2024.55.008684.
Siegel MD, Mark D. 2024a. “UpToDate.” https://www.uptodate.com/contents/acute-respiratory-distress-syndrome-clinical-features-diagnosis-and-complications-in-adults.
Siegel MD, Mark D. 2024b. “UpToDate.” https://www.uptodate.com/contents/acute-respiratory-distress-syndrome-clinical-features-diagnosis-and-complications-in-adults.
The Latest Drowning Statistics.