Introduction
Strabismus, a visual disorder characterized by misalignment of the eyes, results from a lack of coordination in ocular alignment, causing the eyes to fail to focus on the same point in visual space. This misalignment disrupts binocular vision and significantly affects the patient’s quality of visual perception. The global prevalence of strabismus ranges from 2-5% in the general population, with slightly higher rates among children, notably affecting 3-4% of preschool-aged individuals. Typically, strabismus is identified during routine medical examinations or when parents notice an asymmetry in their child’s eye alignment. (1)
The etiology of strabismus encompasses a variety of factors, including both genetic predispositions and acquired causes such as neuromuscular disorders or trauma affecting cranial nerves or extraocular muscles. Strabismus can lead to several severe visual complications, notably amblyopia, a visual impairment resulting from inadequate use of the affected eye. Amblyopia necessitates prompt diagnosis and treatment to prevent adverse effects on visual perception and maintain the patient’s quality of life.
Early intervention in strabismus is crucial for supporting optimal visual development in children. Balanced visual stimulation between the eyes is essential for the development of proper binocular vision and the effective integration of visual information by the brain. Moreover, timely treatment helps prevent significant complications such as permanent visual impairment or persistent diplopia (double vision).
Case Presentation
Patient Data:
- Age and gender: Male patient, 14 years old.
Main Symptoms
- Right eye deflects upward, especially when focusing on nearby objects.
- Double vision, with difficulty focusing on all directions. Resistance with a defective head position.
- The patient did NOT complain of pain or redness in the eye.
- Onset of symptoms: Symptoms began at age 3, with a gradual worsening of symptoms and increased deviation over time.
Clinical Examination
Visual Acuity
- Right Eye: 9/10
- Left Eye: 10/10
- No clinically significant refractive error was noted.
Alignment of the Eyes
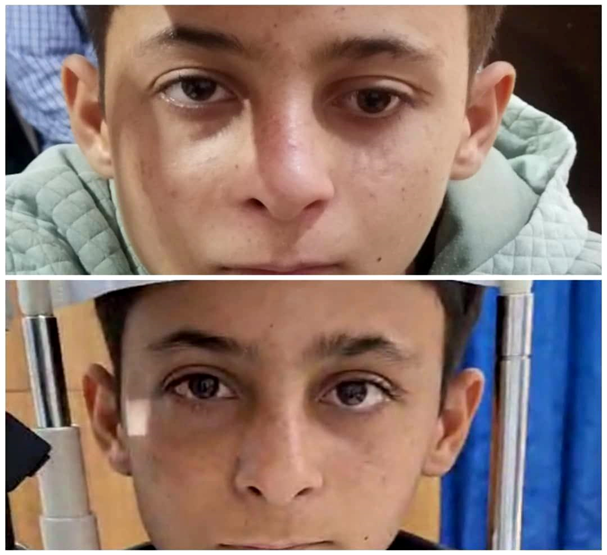
- Right Eye: Hypertropia, particularly noticeable when focusing on nearby objects.
- Head Position: The head tilts towards the right shoulder. The right eye deviates upwards, while the left eye maintains good fixation on the target. When focusing with the right eye, the left eye moves downward to compensate, helping to reduce double vision and alleviate symptoms.
Eye Muscle Examination
- Hyperactivity of the right inferior oblique muscle, while the rest of the extraocular muscles were normal in both eyes.
Additional Examinations
- Examination of the fundus and optic nerve: No abnormalities were observed, indicating the integrity of the posterior structures of the eye.
- No neurological signs were detected.
Coverage checks:
- Vertical deviation was observed, with the right eye showing upward (superior) deviation and the left eye showing downward (inferior) deviation.
Therapeutic procedures
Surgical intervention
Corrective surgery was performed on the right eye that involved shortening the lower misguided muscle to correct its positioning and reduce vertical deviation. The goal of this operation was to restore normal muscular coordination between the eyes and achieve correct alignment, thereby reducing strabismus-related symptoms such as double vision and visual discomfort.
The surgery also involved shortening the length of the muscle to adjust its position and control the angle of movement, which helped adjust the angle of eye movement while looking at different targets. This modification improved the eye’s response to movement and continuously reduced deflection, enhancing accurate alignment in all directions. The surgery was performed under general anesthesia, with preventive measures taken to ensure eye safety and maintain normal blood flow to muscles and nerves.
Complementary therapy
- Visual Exercise Sessions: The exercises included stimulating the affected muscle with the aim of restoring coordination and improving motor control of the eye. These exercises are necessary to enhance the brain’s ability to coordinate between the eyes and enhance bilateral vision.
- Alternating Coverage of the Eyes: Alternating coverage technology was used to enhance the effectiveness of the weaker muscle and improve visual harmony. This technique helps enhance visual fixation and improve the neural response between the eyes.
Follow-up results
Follow up after two months:
- Eye Straightening: Parallel eye alignment was achieved, improving motor coordination and reducing symptoms. The improvement was assessed using the Cover-Uncover test, which confirmed good straightness of both eyes.
- Head Position: The head tilt was resolved, indicating a significant improvement in the balance of ocular function. This improvement was documented using a video assessment of eye movements to monitor posture.
- Visual Ability: There was a clear improvement in visual ability and coordination between the eyes, positively impacting the child’s daily activities such as reading and focusing on nearby objects. This improvement was measured using the Snellen chart.
- Quality of Life: The patient reported an improvement in daily life quality, with a decrease in symptoms related to visual fatigue and double vision.
Case Discussion
Strabismus, also known as “crossed eyes,” is a visual disorder characterized by a misalignment of the eyes, resulting in each eye focusing on different points in space. This lack of coordination can lead to several visual complications, including diplopia (double vision) and amblyopia (lazy eye), particularly if timely intervention is not provided. (2)
Classification of Strabismus
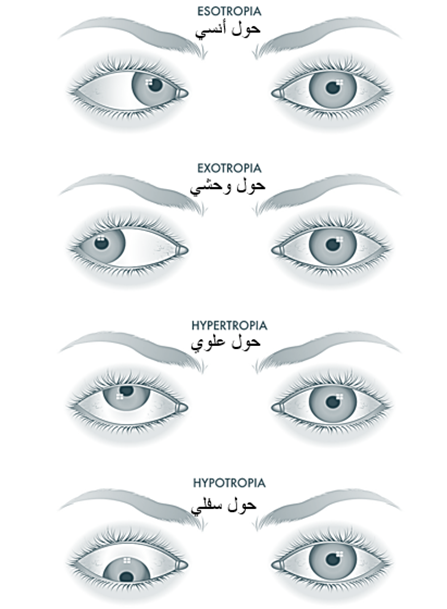
By direction of deviation:
- Esotropia: Inward (medial) deviation of the eye, typically observed when focusing on nearby objects.
- o Exotropia: Outward (lateral) deviation of the eye, often noticeable when looking at distant objects or under stress.
- Vertical Strabismus: Deviation of the eye either upward (hypertropia) or downward (hypotropia).
By temporal pattern
- Intermittent Strabismus: Appears and disappears under certain conditions, such as fatigue or visual strain.
- Constant Strabismus: Persistent misalignment that often requires surgical intervention.
By reason:
- Congenital: It appears in early childhood as a result of genetic factors or birth defects.
- Acquired: Occurs later due to refractive factors, neurological diseases, trauma, or muscle diseases such as myasthenia gravis.
Diagnostic mechanism
History:
- Duration of strabismus, presence of double vision, family history, and use of corrective lenses.
Visual acuity assessment:
- Using a Snellen chart or similar tools.
- Examination of refractive errors with cycloplegic refraction using cyclopentolate 1% administered twice, five minutes apart, followed by examination after 30 minutes.
- Evaluation for the presence of amblyopia.
Strabismus Angle Measurement:
- Cover Test (Cover-Uncover Test): Assesses the presence of a deviation when focusing on a specific target, helping to determine the type of strabismus (esotropia, exotropia, or vertical).
- Alternate Cover Test: Detects latent deviations and assesses the stability of eye alignment by alternately covering each eye without allowing them to fixate together.
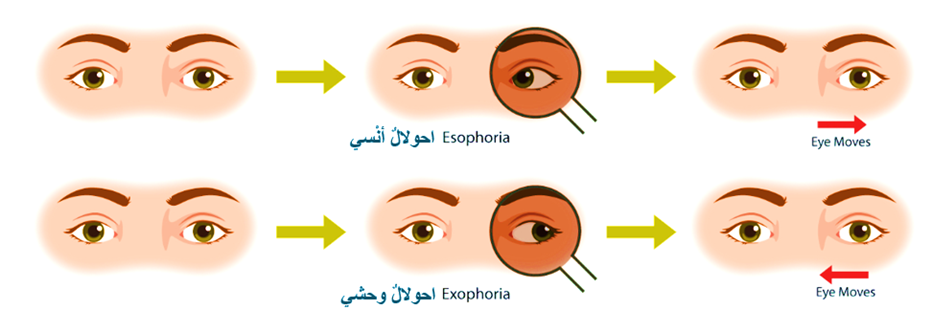
Photo Reflex Tests:
- Hirschberg Test: Assesses the position of the pupils by observing the reflection of light, allowing for an approximate measurement of the strabismus angle.
- Krimsky Test: Uses prisms to accurately measure the angle of deviation by aligning the light reflection symmetrically in both eyes.
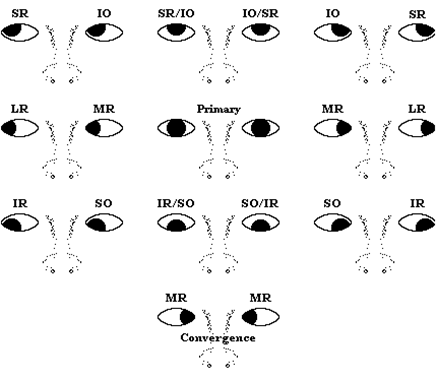
Eye Movement Assessment:
- Evaluates eye muscle function in nine cardinal directions to identify affected muscles and assess nerve integrity. The patient follows a target while head movement is restricted, and eye movement is observed for smoothness, coordination, limitations, or double vision.
Treatment Options
Non-Surgical Treatment:
- Corrective Lenses: Improve vision and reduce deviation by addressing refractive errors.
- Orthoptic Exercises: Aim to enhance coordination between the eyes and strengthen weak muscles.
- Amblyopia Treatment: Involves patching the healthy eye to stimulate and strengthen the affected eye.
Surgical Treatment:
- Muscle Adjustment: Adjusting the length or repositioning of eye muscles to improve alignment and achieve optimal coordination.
Neuropsychological Support:
- Psychological Support: Essential for cases with a neurological basis to reduce psychological impact and enhance self-confidence. Family involvement is recommended to provide ongoing support.
Visual Rehabilitation
- Visual rehabilitation includes a range of therapeutic measures designed to enhance eye function after surgery, including continuous visual exercises aimed at improving neurostimulation and binocular vision. This aspect of treatment is crucial for comprehensive recovery.
Summary
Strabismus, particularly vertical strabismus, is a complex condition that requires early diagnosis and a multidisciplinary treatment approach, including surgical intervention and visual rehabilitation. A combination of early detection, appropriate therapeutic measures, and psychosocial support can significantly improve visual outcomes and overall quality of life. Continuous follow-up is crucial to ensure stability and prevent recurrence. This case highlights the importance of collaboration across medical specialties to provide integrated care, enhancing the patient’s quality of life and minimizing the negative impact of strabismus.
Clarification:
This condition was treated at Bab Al-Hawa Hospital, supported by the Syrian American Medical Society (SAMS) Foundation in June 2024, by the resident doctor in ophthalmology, Dr. Doaa Owaid, under the supervision of the supervising doctor Dr. Ahmed El-Sayed Ali.
References
- Bowling B. Kanski’s Clinical Ophthalmology a Systemic Approach. Vol. 897, Elsevier. 2016.
- Saud A. Foundations of Strabismus | independent [Internet]. 2022. Available from: https://mostaql.com/portfolio/1104995-%D8%A3%D8%B3%D8%B3-%D8%B9%D9%84%D9%85-%D8%A7%D9%84%D8%AD%D9%88%D9%84