Abstract :
Introduction: Kienböck disease is avascular necrosis of the lunate bone in carpal can lead to progressive wrist pain and abnormal carpal motion , diagnosis made with wrist radiographs in advanced cases but may require MRI for detection of early disease. The usual treatment approach is observation and NSAIDs in minimally symptomatic patient , a variety of surgical procedure are available depending on severity of disease and patient’s symptoms .
Case Report: A 25-year-old male with symptomatic Stage III Kienböck’s disease was treated successfully by excision of lunate bone with interposition arthroplasty using a coiled palmaris longus tendon procedure. Observation of the patient 18 months postoperatively, he was relatively pain free and was able to carry out most of his routine activities.
Conclusion: Coiled Palmaris tendon-muscle unit forms a good volume to snugly fit the void created by lunate excision for Grade 4 Kienbock’s disease. However, long-term follow-up is necessary to determine the extent of carpal collapse and functional loss which may occur over time.
Keywords: Kienböck disease, lunate excision, coiled palmaris longus, interposition arthroplasty
Introduction:
Kienböck disease is a rare disease, was described by the Austrian radiologist Robert Kienböck in 1910 as a condition characterized by avascular necrosis of the lunate bone. It is also known as osteonecrosis, lunatomalacia, and aseptic or ischemic necrosis of the lunate.
The lunate is a crescent-shaped carpal bone found within the proximal row of carpal bones. Proximally, it articulates with the radius, with the scaphoid laterally, and with the triquetral medially, and it articulates distally with the capitate, and also articulates on its distal and medial surface with the hamate bone.
The lunate is stabilized by a lateral ligament to the scaphoid and a medial ligament to the triquetrum. l-Ligaments between the radius and carpal bone also stabilize the position of the lunate in the lunate fossa of the radius. The proximal surface of the lunate bone is smooth and convex, articulating with the radius. The lateral surface is flat and narrow, with a crescentic facet for articulation with the scaphoid. The medial surface a smooth and quadrilateral facet for articulation with the triquetral. The palmar surface is rough. The dorsal surface is broad and rounded , The distal surface of the bone is deep and concave.
The lunate receives its blood supply from different arteries, dorsal and palmar branches via dorsal and palmar arteries entering the bone. The blood supply and foramina number is greater in the volar pole than the dorsal pole. Additionally, in about 20% of people, blood supply may arise from palmar vessels only.
The pathophysiology mechanism in this disease is multifactorial and though there is no single definitive cause of kienböck disease and this condition is poorly understood.
Lunate geometry , anatomic variability of lunate blood supply, increased intraosseous pressure from venous stasis, negative ulnar variance, decreased radial inclination, all of this is significant risk factor for development of this condition.
The disease commonly affects the dominant wrist of male manual workers between the age of twenty and forty, although it has a higher incidence in those who have sustained trauma to the wrist, but this is not always present.
The symptoms of Kienböck disease can vary depending on their stage at initial presentation, patients typically present with pain and swilling localized to the radio-lunate facet and classically are insidious in onset and often related to activity, decreased ROM and decreased grip strength in the affected hand and can be present for extended periods before presentation.
Normal value : Radial deviation 15 degree, Ulnar deviation 35 degree, Extension 55 degree, Flexion 65 degree. Supination and pronation approximate 80 degree for both. The average healthy grip strength for men is about 70 pounds
Radiography is the initial imaging technique for assessing Kienböck disease and also can be used to rule out other pathologic conditions, such as arthrosis and fractures. Plain radiography allows the disease to be classified into 4 stages according to Lichtman ; and associates since there are no changes on plain radiography film and Unexplained persistent, non–activity-related dorsal wrist pain in young adult with negative ulnar variance should prompt MRI evaluation, MRI findings in early Kienböck disease include diffuse low-signal intensity throughout lunate on T1 and T2 weighted images. Progressive radiological findings include sclerosis of the lunate, lunate collapse, fixed scaphoid rotation and degeneration of the adjacent intercarpal joints.
Kienbock’s disease progress finally to breakdown of the remaining bones of the hand, so it is a progressive disorder resulting in joint destruction within 3_5 years if untreated, rate of progression is varied from case to case. There is no cure for Kienbock’s disease and remains a challenging clinical problem but prompt treatment can help preserve wrist function and relieve pain. And the decision is often based partially, or even mostly, on the patient’s desire to return to active use of the hand (such as in manual occupations), and the surgeon’s level of expertise with different treatments.
Treatment options also depend upon the severity and stage of the disease and ulnar variance. Various treatment options have been proposed, none of them being proven completely effective. In early stages (stage 1), the treatment can be as simple as observation, activity changes, and/or cast immobilization for 3-month.
For more advanced stages or fail trial of immobilization, surgery is usually considered. Surgery may be done initially moderate stages for lunate preservation, reduce forces across lunate and wrist joint (joint leveling procedures), improve vascularity in lunate (revascularization of lunate) and avoid further fragmentation and collapse by, scapho-trapezio-trapezoid arthrodesis , scapho-capitate arthrodesis , vascularized bone grafting.
When the lunate is severely collapsed or arthritic, salvage treatments such as lunate and other wrist bone removal may be necessary, as lunate resection with replacement its place via vascularized pisiform bone, palmaris longus tendon arthroplasty, prosthetic replacement, and other procedure as proximal row carpectomy and wrist arthrodesis all described.
Case report:
The case was of a 25-year-old male complained of persistent pain in his right wrist particularly with activity, reduced range of motion (ROM), and reduced grip power, 18 months before presentation. The patient had previously fracture around the wrist (unknown exactly), he worked as a carpenter with repetitive use of hammer.
Clinical examination showed marked tenderness over the dorsal aspect of the wrist and limited Flexion/extension of the right wrist compared with the other side due to pain (particularly extension). On standard PA and lateral radiographs and oblique views there is no fracture but the wrist showed a densification of the lunate with a flattened and irregular appearance with negative ulnar variance and without a fixed rotation of the scaphoid or signs of OA .
The diagnosis was made of stage III Kienböck’s disease according to Lichtman classification.

Based on the grade of the disease, we treated the patient surgically by excision of lunate bone with interposition arthroplasty using a coiled palmaris longus tendon .
This surgery is relatively easy, quick and gives good functional results in the short term when taking about the articular function and collapse in the wrist bones.
One of the main reasons for choosing this method is the patient’s rejection of other treatment methods that include excision or arthrodesis of the proximal row carpal bones and the importance of a quick return to work for the patient.
In addition, since our area in the NW Syria – Aleppo, we are unable to use other more expensive surgical methods, and we rely on using faster and less expensive surgeries, (this is due to the war conditions) with the absence of the means used in other methods, such as wrist fusion plate or silicone implants and this method does not prevent in the future from Using other methods when failure or other possibilities are available .
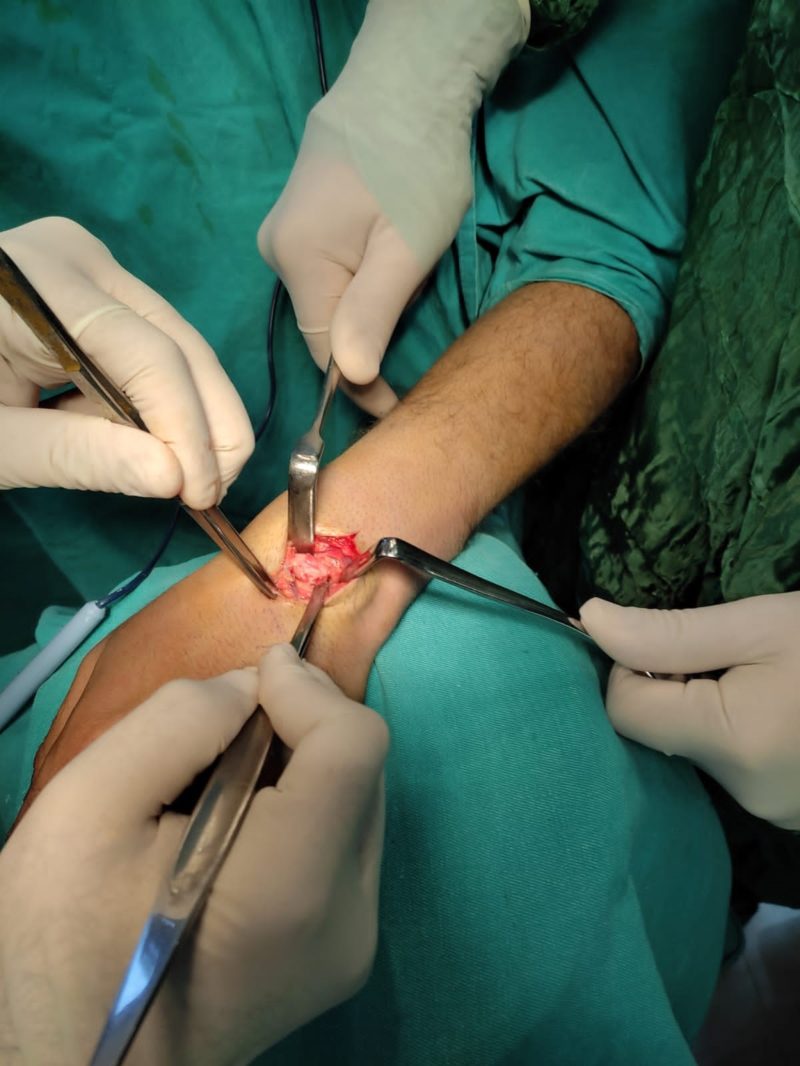
Using a palmar approach under regional anesthesia, the palmar incision used to excise the lunate bone, the it was extended proximally and the palmaris longus muscle was identified and detached from its origin, keeping the insertion of the palmaris longus tendon intact. The muscle belly along with the tendon was coiled and placed into the void created by the excision of lunate , Since tendon and muscle belly rolled combined formed a good size roll, it fitted snuggly in the void and we felt no need for temporary K wire fixation. Postoperatively, wrist was immobilized in a cast for four weeks. The lunate bone can also be removed through dorsal approach , as shown in the pictures:

Patient subsequently underwent physical therapy to improve strength and range of motion of wrist.
18 months postoperatively, the patient was relatively pain free and was able to carry out most of his routine activities.
The radiograph at final follow-up showed no carpal collapse
Final ROM: Radial deviation 10 degree, ulnar deviation 25 degree, extension 40 degree, flexion 35 degree. Supination and pronation approximate 60 degree for both. After surgery, the grip strength was about half of normal and near-normal strength was restored with physical therapy.


Excision of lunate recommended for late stage Kienbock’s disease which results in pain relief and functional improvement. However, filling the void with a coiled tendon after excision of the lunate is recommended to prevent carpal collapse. Silicone replacement arthroplasty , vascularized pisiform transposition and coiled tendon grafts are current methods of filling the void. Silicone replacement arthroplasty increases the cost involved in the procedure and the results are not encouraging due to silicone synovitis and subsequent carpal collapse. Interposition arthroplasty with a biological material like transposed vascularized pisiform (Saffars procedure) have also been described .
However, this procedure is technically difficult when compared to interposition arthroplasty using a coiled tendon. Coiled tendon grafts are currently the procedure of choice and Palmaris longus tendon is preferred as the graft can be harvested through the same incision.
One major issue with palmaris longus tendon is that the volume is often insufficient. The snug fitting of the tendon-muscle roll will prevents early collapse and hence no K wire fixation was used in this case. At 18 months follow up no obvious carpal collapse supports our theory.

CONCLUSION :
Definite treatment of late stage of Kienbock’s disease remains controversial. The ideal procedure should relieve the pain and maintain normal wrist function as much as possible. Excision of the lunate bone in the late stages of Kienbock’s disease relieves the pain. To maintain grip strength, increase range of motion, and prevent carpal collapse, this space has been filled with tendon, fascia, and various materials such as steel, ivory, silicone, and PyroCarbon .
Late stage Kienbock’s disease can be successfully treated with lunate excision and interposition arthroplasty using the ipsilateral coiled palmaris longus tendon and muscle belly to give excellent functional results in the short-term. It should be noted that this method is universal and not innovative.
The results in our case were compared with the results of cases treated in the same way. It shows success in the short and medium term. Some of these report cases from which we have quoted have been mentioned in the references.
CLINICAL MESSAGE :
Coiled Palmaris tendon-muscle unit forms a good volume to snugly fit the void created by lunate excision for Grade 4 Kienbock’s disease. This large volume and snug fit is enough to avoid carpal collapse and may not require temporary K wire fixation.
Short term follow up of use of this technique in single patient has shown good result. However, long-term follow-up is necessary to determine the extent of carpal collapse and functional loss which may occur over time.
Supervising Doctor : Dr. Rfa’at Bitar
Dr.zohair alabdullah / Alrrahma
Darkush hospital
Reference :
- Kienbock’s Disease treated with Interposition Arthroplasty using Ipsilateral Palmaris Longus Tendon and Muscle Belly
- Tendon interposition and ligament reconstruction with ECRL tendon in the late stages of Kienböck’s disease: a cadaver study
- https://www.orthobullets.com/hand/6050/kienbocks-disease
- Miller’s Review of Orthopaedic 7th Edition