Introduction
Acute pancreatitis is a severe inflammatory condition of the pancreas that may cause serious complications such as secondary peritonitis. This article is about a case of secondary peritonitis caused by hyperlipidic pancreatitis, which is relatively rare compared to other complications of acute pancreatitis. The resident doctors of the Syrian Commission for Medical Specializations have succeeded in managing this case under the supervision of specialist doctors at Sham Specialized Hospital for Internal Diseases, which is supported by the Sham Humanitarian Organization, and in this article we will discuss how to deal with and manage this case.
View Status
Clinical Story:
Mrs. M.C., a 21-year-old mother of five, was presented to the emergency department with a sudden onset of acute abdominal pain in the epigastric region, radiating to the hypochondria, accompanied by multiple episodes of vomiting. She has no history of medical treatment but has undergone three previous caesarean sections. Notably, the patient reported a family history of hyperlipidemia, which led to the deaths of her sister and uncle.
Upon clinical examination, she was found to be pale, with cold sweats, and experiencing generalized abdominal pain, most severe in the epigastric region.
Vital signs:
- Blood pressure: 110/70 mm Hg
- Pulse: 130 beats / min
- Oxygen saturation: 94%
Laboratory results:
Upon acceptance:
- Amylase: 340 units/L
- Triglycerides: 1300 mg/dL
- Cholesterol: 640 mg/dL
- Urea /Urinate: 58 mg/dL
- Blood sugar: 205 mg/dL
- Sodium: 136 mmol/L
- Potassium: 3.8 mmol/L
- Calcium isomy: 1.4 mmol/L
The patient was diagnosed with acute hyperlipidemia pancreatitis.
Measure:
The patient was admitted to the ICU with the following treatment plan:
- Intravenous rehydration (30 ml/kg for the first three hours) and then 125 ml/h with urinary outgoing / IVC monitoring.
- Symptomatic treatment
- Omeprazole 40 mg
- Acetaminophen / Paracetamol 1g
- Ondansetron 8 mg
- Protective dilution:
- Enoxaparin 0.4 ml
- Continuous fast insulin pump (5 units/hour).
- Antilipid-lowering treatment (Fenofibrate 300 mg twice daily).
- Potassium replacement at the rate of 40 mcg per liter (to avoid potassium drop by the effect of insulin).
- Compensate 1g calcium gluconate.
- Sugar serum 10% adjusted to 50 ml/h to avoid hypoglycemia.
The next day, IV rehydration was reduced to 100 ml/h with the rest of the treatment plan continued.
With daily triglyceride level monitoring + electrolyte monitoring.
Complications and subsequent management:
On the next day, the patient’s condition worsened, developing palpitations and dyspnea at rest, with intensified abdominal pain. Vital signs indicated a pulse of 180 beats per minute, and supraventricular tachycardia (SVT) was confirmed by electrocardiogram. She was treated with 6 mg of intravenous adenosine and 25 mg of metoprolol administered twice daily.
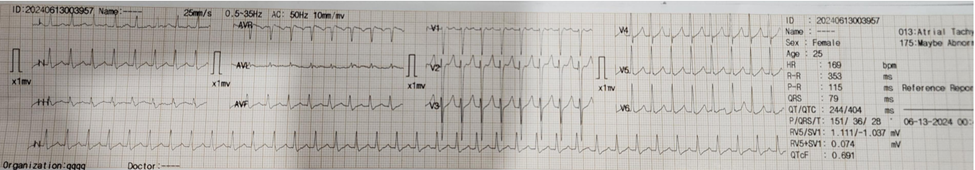
Electrocardiogram tachycardiogram 175
Echocardiography:
- Mild pericardial effusion
- Bilateral pleural effusion, more severe on the right side
- Light ascites
Laboratory tests:
- Additional rise in triglycerides (2300 mg/dL).
Management:
- Increased the dose of the insulin pump to 8 units/hour.
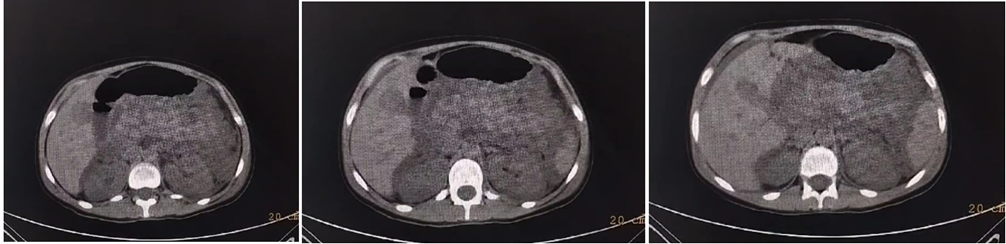
- Conducted a computerized tomography (CT) scan of the abdomen with contrast, which revealed:
- Comprehensive pancreatitis and edema
- Generalized pancreatic edema, most severe in the tail
- Accumulated fluid within the abdomen
- Diagnostic paracentesis confirmed the presence of secondary peritonitis:
- WBC 4800
- T.p 3.3
- 2.5
- Amylase 317
- LDH 1950
A general surgery consultation was requested to rule out any surgical causes, and it was determined that immediate surgical intervention was not required. Antibiotic treatment with Meropenem 1g three times daily was initiated, and the insulin pump was continued until triglyceride levels dropped below 500 mg/dL.
The patient experienced recurrent SVT episodes that did not respond to drug therapy and were accompanied by a drop in arterial pressure (80/40 mmHg). This necessitated synchronized cardioversion at 100 joules, successfully restoring sinus rhythm with a heart rate of 90 beats per minute.
Result:
The patient showed significant clinical and laboratory improvement after about 14 days of treatment and observation:
- Blood glucose levels stabilized within normal limits
- Decline in inflammatory markers
- Receding abdominal pain
- Reduction in blood lipid levels to 250 mg/dL
The patient was discharged with oral lipid-lowering therapy (Fenofibrate 300 mg once daily) and continued antibiotic treatment.
Follow-up in the gastroenterology clinic indicated functional stability without complications.
Conclusion
Young patients with severe hyperlipidemia and pancreatitis require multidisciplinary management to achieve successful results. Early detection and immediate intervention can significantly improve outcomes, even in the presence of significant complications.
Early secondary peritonitis due to acute hyperlipidemia pancreatitis: the silent threat
Most doctors can distinguish acute pancreatitis caused by gallstones or excessive alcohol intake. However, an equally rare and serious complication is acute hyperlipidemic pancreatitis (AHP), which can lead to early secondary peritonitis. This condition necessitates rapid identification and intervention. (1)
Definition and challenges
Acute hyperlipidemic pancreatitis is a severe form of pancreatitis caused by elevated triglyceride levels in the blood. This elevation can result in intense inflammation of the pancreas, leading to severe abdominal pain, nausea, and vomiting. The condition can deteriorate rapidly, necessitating urgent medical intervention to prevent serious complications such as early secondary peritonitis.
The importance of rapid diagnosis
Hyperlipidemia is a rare yet significant etiological factor in pancreatitis, capable of precipitating cyclic ascites and peritonitis upon extension of pancreatic inflammation to the peritoneum – the lining of the abdominal cavity. Inflammation of the peritoneum can lead to bacterial infection and rapid dissemination, culminating in a life-threatening condition. Therefore, timely diagnosis and intervention are crucial to mitigate the progression of severe symptoms and associated complications. (2)
In cases of acute hyperlipidemic pancreatitis, serum levels of amylase and lipase may remain within normal ranges or exhibit only marginal elevation, posing challenges to diagnosis. Patients commonly present with intense abdominal pain, nausea, vomiting, and flatulence. Physical examination may reveal abdominal tenderness and mobile dullness upon percussion.
Diagnostic imaging plays a pivotal role in confirming the diagnosis. Ultrasonography can identify ascites, while contrast-enhanced CT scans reveal inflammatory changes surrounding the pancreas characteristic of acute pancreatitis. Analysis of ascitic fluid typically shows a milky appearance with elevated triglyceride levels, confirming the presence of chylous ascites.
Pathophysiological
The pathophysiological mechanism underlying acute pancreatitis in the context of hyperlipidemia involves several key steps:
- Elevated Triglyceride Levels: High levels of triglycerides lead to the formation of triglyceride-rich lipoproteins, particularly chylomicrons.
- Hydrolysis and Release of Free Fatty Acids (FFAs): Chylomicrons undergo hydrolysis in the pancreatic vascular bed, liberating significant amounts of free fatty acids (FFAs).
- Toxic Effect of FFAs: Excess FFAs overwhelm the binding capacity of plasma albumin, resulting in the formation of toxic FFA complexes.
- Cellular Damage: These toxic FFA complexes can induce cellular injury, particularly affecting pancreatic acinar cells, platelets, and vascular endothelium.
- Ischemia and Acidosis: The accumulation of toxic FFAs leads to local ischemia within the pancreas and contributes to tissue acidosis.
- Activation of Enzymes: Acidosis and local tissue damage trigger activation of pancreatic enzymes, including trypsinogen.
- Inflammation and Pancreatic Injury: Activated enzymes, particularly trypsinogen, initiate autodigestion of pancreatic tissue, leading to inflammation and necrosis characteristic of acute pancreatitis.
- Peritoneal Complications: In severe cases, the release of pancreatic enzymes and inflammatory mediators can lead to acute peritonitis, sometimes manifesting as chylous ascites, a rare but serious complication.
Understanding these steps helps in comprehending how hyperlipidemia can precipitate acute pancreatitis through the complex interplay of lipid metabolism, enzymatic activation, and inflammatory responses within the pancreas and surrounding tissues. (3)
Recognizing Signs and Symptoms
Diagnosing early secondary peritonitis can pose challenges due to its symptoms overlapping with other conditions. Nevertheless, clinicians should be vigilant for the following indicative signs:
- Severe abdominal pain exacerbated by movement or palpation
- Abdominal swelling or distention
- Fever accompanied by chills
- Nausea and vomiting
- – Decreased appetite
Diagnosis and Treatment
Diagnosing early secondary peritonitis typically necessitates a multifaceted approach involving:
- Physical Examination: Assessing signs of abdominal tenderness, distension, and guarding.
- Imaging Tests: Such as CT scans, which can reveal signs of peritoneal inflammation, fluid collections, or perforation.
- Blood Tests: Including complete blood count (CBC) and inflammatory markers like C-reactive protein (CRP) to assess for signs of infection and inflammation.
This comprehensive evaluation helps clinicians to promptly identify and manage secondary peritonitis, crucial for minimizing complications and improving patient outcomes.
Management of acute pancreatitis with hyperlipidemia:
Early management of acute pancreatitis with hyperlipidemia involves a structured approach aimed at mitigating inflammation, managing complications, and optimizing patient outcomes:
- Initial Conservative Treatment: This includes hospitalization for close monitoring, initiation of intravenous rehydration to maintain fluid and electrolyte balance, bowel rest to reduce pancreatic stimulation, and effective pain management.
- Targeted Treatments: Lowering triglyceride levels is pivotal. This can be achieved through interventions such as heparin therapy to enhance lipoprotein lipase activity, insulin to suppress hepatic triglyceride production, and lipid-lowering agents like fibrates or statins.
- Plasmapheresis: Reserved for severe cases where conventional therapies
- Supportive Care: Includes fat-free parenteral nutrition to prevent exacerbation of pancreatic inflammation and advanced supportive measures like hemoperfusion to remove inflammatory mediators.
- Surgical Intervention: Indicated for specific complications such as infected pancreatic necrosis, pseudocysts, or persistent organ failure despite medical management.
Early diagnosis facilitated by clinical suspicion and confirmatory tests, along with prompt initiation of appropriate treatment strategies, are paramount in improving patient prognosis and reducing the risk of complications associated with acute pancreatitis secondary to hyperlipidemia.(4)
Useful Conclusion:
Early secondary peritonitis caused by acute pancreatitis caused by high lipidemia is a serious condition that requires quick and decisive action. By understanding symptoms and seeking immediate medical care, we can improve outcomes and prevent life-threatening complications. As healthcare providers and individuals, awareness and vigilance are key to managing this condition effectively.
This case was managed by the resident doctors of the Syrian Board of Medical Specializations:
Dr. Heba Ateeq, Dr. Abdel Aleem Al-Bakour, Dr. Ali Al-Daif
Under the supervision of specialists: Dr. Khaled Al-Marei, Dr. Abdul Rahman Suleiman, Dr. Musab Al-Ibrahim
At Sham Specialized Hospital for Internal Diseases, supported by Sham Humanitarian Organization.
- Diagnostic paracentesis confirmed the presence of secondary peritonitis:
- WBC 4800
- T.p 3.3
- 2.5
- Amylase 317
- LDH 1950
A general surgery consultation was requested to rule out any surgical causes, and it was determined that immediate surgical intervention was not required. Antibiotic treatment with Meropenem 1g three times daily was initiated, and the insulin pump was continued until triglyceride levels dropped below 500 mg/dL.
The patient experienced recurrent SVT episodes that did not respond to drug therapy and were accompanied by a drop in arterial pressure (80/40 mmHg). This necessitated synchronized cardioversion at 100 joules, successfully restoring sinus rhythm with a heart rate of 90 beats per minute.
Result:
The patient showed significant clinical and laboratory improvement after about 14 days of treatment and observation:
- Blood glucose levels stabilized within normal limits
- Decline in inflammatory markers
- Receding abdominal pain
- Reduction in blood lipid levels to 250 mg/dL
The patient was discharged with oral lipid-lowering therapy (Fenofibrate 300 mg once daily) and continued antibiotic treatment.
Follow-up in the gastroenterology clinic indicated functional stability without complications.
Conclusion
Young patients with severe hyperlipidemia and pancreatitis require multidisciplinary management to achieve successful results. Early detection and immediate intervention can significantly improve outcomes, even in the presence of significant complications.
Early secondary peritonitis due to acute hyperlipidemia pancreatitis: the silent threat
Most doctors can distinguish acute pancreatitis caused by gallstones or excessive alcohol intake. However, an equally rare and serious complication is acute hyperlipidemic pancreatitis (AHP), which can lead to early secondary peritonitis. This condition necessitates rapid identification and intervention. (1)
Definition and challenges
Acute hyperlipidemic pancreatitis is a severe form of pancreatitis caused by elevated triglyceride levels in the blood. This elevation can result in intense inflammation of the pancreas, leading to severe abdominal pain, nausea, and vomiting. The condition can deteriorate rapidly, necessitating urgent medical intervention to prevent serious complications such as early secondary peritonitis.
The importance of rapid diagnosis
Hyperlipidemia is a rare yet significant etiological factor in pancreatitis, capable of precipitating cyclic ascites and peritonitis upon extension of pancreatic inflammation to the peritoneum – the lining of the abdominal cavity. Inflammation of the peritoneum can lead to bacterial infection and rapid dissemination, culminating in a life-threatening condition. Therefore, timely diagnosis and intervention are crucial to mitigate the progression of severe symptoms and associated complications. (2)
In cases of acute hyperlipidemic pancreatitis, serum levels of amylase and lipase may remain within normal ranges or exhibit only marginal elevation, posing challenges to diagnosis. Patients commonly present with intense abdominal pain, nausea, vomiting, and flatulence. Physical examination may reveal abdominal tenderness and mobile dullness upon percussion.
Diagnostic imaging plays a pivotal role in confirming the diagnosis. Ultrasonography can identify ascites, while contrast-enhanced CT scans reveal inflammatory changes surrounding the pancreas characteristic of acute pancreatitis. Analysis of ascitic fluid typically shows a milky appearance with elevated triglyceride levels, confirming the presence of chylous ascites.
Pathophysiological
The pathophysiological mechanism underlying acute pancreatitis in the context of hyperlipidemia involves several key steps:
- Elevated Triglyceride Levels: High levels of triglycerides lead to the formation of triglyceride-rich lipoproteins, particularly chylomicrons.
- Hydrolysis and Release of Free Fatty Acids (FFAs): Chylomicrons undergo hydrolysis in the pancreatic vascular bed, liberating significant amounts of free fatty acids (FFAs).
- Toxic Effect of FFAs: Excess FFAs overwhelm the binding capacity of plasma albumin, resulting in the formation of toxic FFA complexes.
- Cellular Damage: These toxic FFA complexes can induce cellular injury, particularly affecting pancreatic acinar cells, platelets, and vascular endothelium.
- Ischemia and Acidosis: The accumulation of toxic FFAs leads to local ischemia within the pancreas and contributes to tissue acidosis.
- Activation of Enzymes: Acidosis and local tissue damage trigger activation of pancreatic enzymes, including trypsinogen.
- Inflammation and Pancreatic Injury: Activated enzymes, particularly trypsinogen, initiate autodigestion of pancreatic tissue, leading to inflammation and necrosis characteristic of acute pancreatitis.
- Peritoneal Complications: In severe cases, the release of pancreatic enzymes and inflammatory mediators can lead to acute peritonitis, sometimes manifesting as chylous ascites, a rare but serious complication.
Understanding these steps helps in comprehending how hyperlipidemia can precipitate acute pancreatitis through the complex interplay of lipid metabolism, enzymatic activation, and inflammatory responses within the pancreas and surrounding tissues. (3)
Recognizing Signs and Symptoms
Diagnosing early secondary peritonitis can pose challenges due to its symptoms overlapping with other conditions. Nevertheless, clinicians should be vigilant for the following indicative signs:
- Severe abdominal pain exacerbated by movement or palpation
- Abdominal swelling or distention
- Fever accompanied by chills
- Nausea and vomiting
- – Decreased appetite
Diagnosis and Treatment
Diagnosing early secondary peritonitis typically necessitates a multifaceted approach involving:
- Physical Examination: Assessing signs of abdominal tenderness, distension, and guarding.
- Imaging Tests: Such as CT scans, which can reveal signs of peritoneal inflammation, fluid collections, or perforation.
- Blood Tests: Including complete blood count (CBC) and inflammatory markers like C-reactive protein (CRP) to assess for signs of infection and inflammation.
This comprehensive evaluation helps clinicians to promptly identify and manage secondary peritonitis, crucial for minimizing complications and improving patient outcomes.
Management of acute pancreatitis with hyperlipidemia:
Early management of acute pancreatitis with hyperlipidemia involves a structured approach aimed at mitigating inflammation, managing complications, and optimizing patient outcomes:
- Initial Conservative Treatment: This includes hospitalization for close monitoring, initiation of intravenous rehydration to maintain fluid and electrolyte balance, bowel rest to reduce pancreatic stimulation, and effective pain management.
- Targeted Treatments: Lowering triglyceride levels is pivotal. This can be achieved through interventions such as heparin therapy to enhance lipoprotein lipase activity, insulin to suppress hepatic triglyceride production, and lipid-lowering agents like fibrates or statins.
- Plasmapheresis: Reserved for severe cases where conventional therapies
- Supportive Care: Includes fat-free parenteral nutrition to prevent exacerbation of pancreatic inflammation and advanced supportive measures like hemoperfusion to remove inflammatory mediators.
- Surgical Intervention: Indicated for specific complications such as infected pancreatic necrosis, pseudocysts, or persistent organ failure despite medical management.
Early diagnosis facilitated by clinical suspicion and confirmatory tests, along with prompt initiation of appropriate treatment strategies, are paramount in improving patient prognosis and reducing the risk of complications associated with acute pancreatitis secondary to hyperlipidemia.(4)
Useful Conclusion:
Early secondary peritonitis caused by acute pancreatitis caused by high lipidemia is a serious condition that requires quick and decisive action. By understanding symptoms and seeking immediate medical care, we can improve outcomes and prevent life-threatening complications. As healthcare providers and individuals, awareness and vigilance are key to managing this condition effectively.
This case was managed by the resident doctors of the Syrian Board of Medical Specializations:
Dr. Heba Ateeq, Dr. Abdel Aleem Al-Bakour, Dr. Ali Al-Daif
Under the supervision of specialists: Dr. Khaled Al-Marei, Dr. Abdul Rahman Suleiman, Dr. Musab Al-Ibrahim
At Sham Specialized Hospital for Internal Diseases, supported by Sham Humanitarian Organization.
- Chylous ascites secondary to hyperlipidemic pancreatitis with normal serum amylase and lipase, Chylous ascites secondary to hyperlipidemic pancreatitis with normal serum amylase and lipase – PMC (nih.gov)
- Acute chylous peritonitis due to acute pancreatitis, Acute chylous peritonitis due to acute pancreatitis – PMC (nih.gov)
- Hypertriglyceridemic pancreatitis: Epidemiology, pathophysiology and clinical management, Hypertriglyceridemic pancreatitis: Epidemiology, pathophysiology and clinical management – PMC (nih.gov)
- Management of Acute Severe Hyperlipidemic Pancreatitis, (PDF) Management of Acute Severe Hyperlipidemic Pancreatitis (researchgate.net)

