Summary
Pulmonary embolism is a life-threatening medical condition characterized by severe blockage of the pulmonary arteries that can sometimes cause obstructive shock. Rapid diagnosis and decisive treatment are key factors for patient survival. This report details a successful management by a resident physician at the Syrian Board of Medical Specialization (SBOMS) of a 60-year-old patient who developed symptoms of pulmonary embolism and obstructive shock and was successfully treated at SAMS-supported Bab Al-Hawa Hospital.
Patient Information
A 60-year-old female patient, referred to as A.A., presented to the Bab Al-Hawa Hospital clinics with symptoms of chest discomfort, dyspnea, epigastric abdominal pain, food vomiting, fever, and chills. Her medical history includes hypertension and a cardiac catheterization performed three days prior to her visit.
Clinical examination
During the initial assessment, the patient was found to be conscious and responsive, exhibiting pallor and sweating, and experiencing respiratory distress at rest without cyanosis.
Clinical examination revealed the following findings:
– Chest: Soft rales at the bases of the lungs, with supraclavicular retraction and sternal pull.
– Cardiovascular: Regular and rapid heart sounds (S1 and S2).
– Abdomen: Soft and non-tender, with no palpable organomegaly.
– Extremities: Generalized edema and localized warmth in the lower right limb, with signs indicative of deep vein thrombosis (DVT).
Vital signs:
- Blood pressure: 60/30 mmHg
- Pulse: 102 beats per minute
- Oxygenation: 88% on room air
- Temperature: 37.3°C
- Respiratory rate: twenty-two breaths per minute
- Urine output: Spontaneous and unmeasured
Investigations
Preliminary Laboratory and Imaging Results:
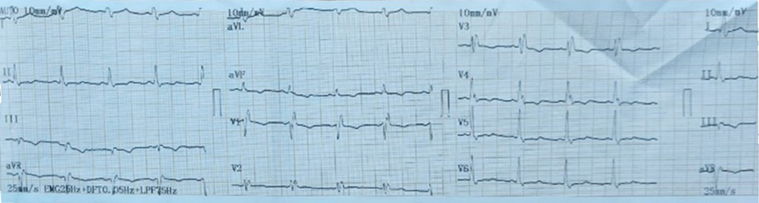
- ECG: Right heart blockade (indicative of old changes)
- Chest X-ray: Within normal limits
- Laboratory Results:
- Leukocytes: 11,000/mm³
- Hemoglobin: 10.3 g/dL
- Platelets: 81,000/mm³
- Glucose: 249 mg/dL
- C-reactive protein (CRP): 14 mg/L
- Blood urea nitrogen (BUN): 65 mg/dL
- Creatinine: 2.4 mg/dL
- Troponin: Negative
- Chest X-ray: Within normal limits.
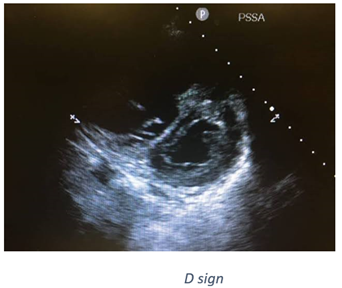
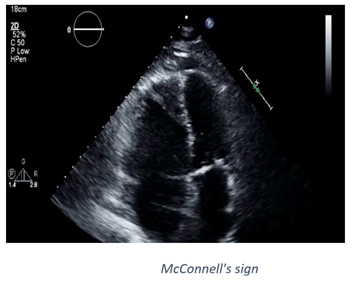
- Echocardiogram:
- Significant dilation of the right atrium and right ventricle.
- Severe tricuspid regurgitation with a pulmonary systolic pressure of 50 mm Hg.
- Presence of a “D sign,” indicating right ventricular strain.
Wells Criteria: According to the Wells criteria for assessing the likelihood of pulmonary embolism, the probability was high, with a score of 7.5.

- Doppler Ultrasound of Lower Limb Veins:
- Obstruction with hypoechoic thrombosis in the femoral vein, indicating acute or subacute phase thrombosis.
- Thrombosis in the popliteal vein.
- No evidence of superficial varicose veins.
- Result indicative of deep vein thrombosis (DVT).
- Doppler Ultrasound of Lower Limb Arteries:
- A false aneurysm in the lower right limb at the level of the common femoral artery, measuring 25 mm.
- – The rest of the arteries appeared normal.
Diagnosis and treatment
Based on the clinical symptoms, signs, and laboratory findings, the patient was diagnosed with pulmonary embolism accompanied by obstructive shock. Computed tomography (CT) of the chest with contrast was avoided due to the deterioration of kidney function and the instability of the hemodynamic state. Treatment for pulmonary embolism was initiated with a loading dose of heparin, followed by thrombolytic therapy according to the appropriate protocol, and the patient was placed on cardiac support.
Results and follow-up
Two hours after the administration of streptokinase, the patient demonstrated significant clinical improvement, with the resolution of respiratory distress and enhanced oxygenation. The vital signs were as follows:
- Blood pressure: 110/60 mmHg
- Pulse: 85 beats per minute
- Oxygenation: 93% on room air
The following day, a cardiac echocardiogram revealed:
- Reduction in the dilation of the right atrium and right ventricle
- Mild tricuspid regurgitation
- Pulmonary artery systolic pressure 25 mm Hg
An Echo Doppler of the right lower limb showed:
- Presence of a thrombus in the common femoral vein
- A false aneurysm at the level of the common femoral artery
The case was subsequently managed by a vascular specialist.
After two days of stabilization and observation, the patient was discharged in good health.
Discussion
1. Challenges in diagnosis
A primary challenge encountered in this case was the elevated creatinine level, which precluded the use of thoracic CT scan. Nevertheless, leveraging cardiac echocardiography and lower peripheral vein eco-Doppler proved adequate to confirm the diagnosis and formulate an effective treatment strategy.
2. Lessons learned
Emphasizing the integration of clinical symptoms with available diagnostic modalities can suffice to diagnose critical pulmonary embolism, even in instances where advanced testing is unavailable.
Pulmonary Embolism
The diagnosis of pulmonary embolism (PE), a critical medical emergency characterized by the abrupt obstruction of a pulmonary artery or its branches by a blood clot, air, or fat, involves a multifaceted approach encompassing clinical symptoms, physical examination findings, laboratory analyses, and imaging studies. In the case under consideration, symptoms such as dyspnea and chest pain radiating to the back, coupled with mediastinal enlargement observed on chest radiography, raised suspicion for pulmonary embolism. However, the patient’s elevated creatinine levels precluded the administration of intravenous contrast material for chest CT scans, typically considered the diagnostic gold standard for pulmonary embolism detection.
Clinical signs and symptoms
The hallmark symptom of pulmonary embolism is typically sudden-onset dyspnea, often accompanied by pleuritic chest pain. Additional manifestations may include syncope, hemoptysis, gastrointestinal symptoms, and signs of Deep Venous Thrombosis (DVT). The presentation can vary widely depending on factors such as thrombus size, degree of pulmonary vascular obstruction, and the patient’s overall health.
Diagnosis
Pulmonary embolism is typically diagnosed through a blend of clinical probability assessment and diagnostic examinations. Clinical probability is gauged using scoring systems such as the Wells or Geneva criteria, which evaluate the probability of pulmonary embolism by considering the patient’s symptoms, physical signs, and predisposing risk factors.
Diagnostic tests
- In cases of high clinical probability, treatment with heparin anticoagulation is initiated, and the patient undergoes a chest CT scan utilizing the Embolus protocol.
- – For patients with low or moderate clinical probability, a D-dimer analysis is conducted. If the D-dimer levels are elevated, the patient is referred for a chest CT scan employing the embolic protocol.
Therapy
Treatment for pulmonary embolism usually involves anticoagulant therapy with heparin or warfarin to prevent further clotting. In severe cases, it may be necessary to dissolve the thrombus to dissolve the clot. The protocol for applying streptokinase, a clotting agent, includes an initial dose of 1.5 million IU within two hours or 250,000 IU over half an hour, followed by 100,000 IU per hour for 12-24 hours.
Risk factors
Pulmonary embolism tends to be more prevalent among individuals with specific predisposing factors, which include:
- Prolonged hospitalization or bed rest for an extended duration.
- Extended periods of immobility during airplane, car, or train travel without adequate movement.
- Severe trauma resulting in a broken leg or other major injuries.
- Undergoing hip or knee replacement surgery.
- Utilization of intravenous catheters.
- Presence of cancer or undergoing chemotherapy treatment.
- Pregnancy or use of oral contraceptives.
- Obesity.
- Smoking.
- Use of hormone replacement therapy.
- Pre-existing conditions such as heart failure or severe chronic lung disease.
- Inflammatory bowel disease.
- Presence of a prothrombotic state, characterized by an increased tendency for blood clot formation.
Prevention
Preventive measures for pulmonary embolism encompass various strategies, including:
- Encouraging increased limb mobility, particularly during extended periods of immobility.
- Administration of medications aimed at preventing blood clot formation.
- Utilization of compression stockings to facilitate blood flow and reduce the risk of clot formation.
Disclaimer:
This case was received and managed by the two internal medicine residents: Dr. Omar Hilal and Dr. Bassel Murad, and the cardiologist Dr. Ahmed Al-Omar at Bab Al-Hawa Hospital, the Department of Internal Medicine Clinics supported by Sams and accredited to train residents of the Syrian Board of Medical Specializations (SBOMS).

